Data-driven analytics
Offering superior value-based care and payment integrity.

A healthcare data analytics hub can drive superior outcomes and increase competitive advantage
Aggregate and act on day one
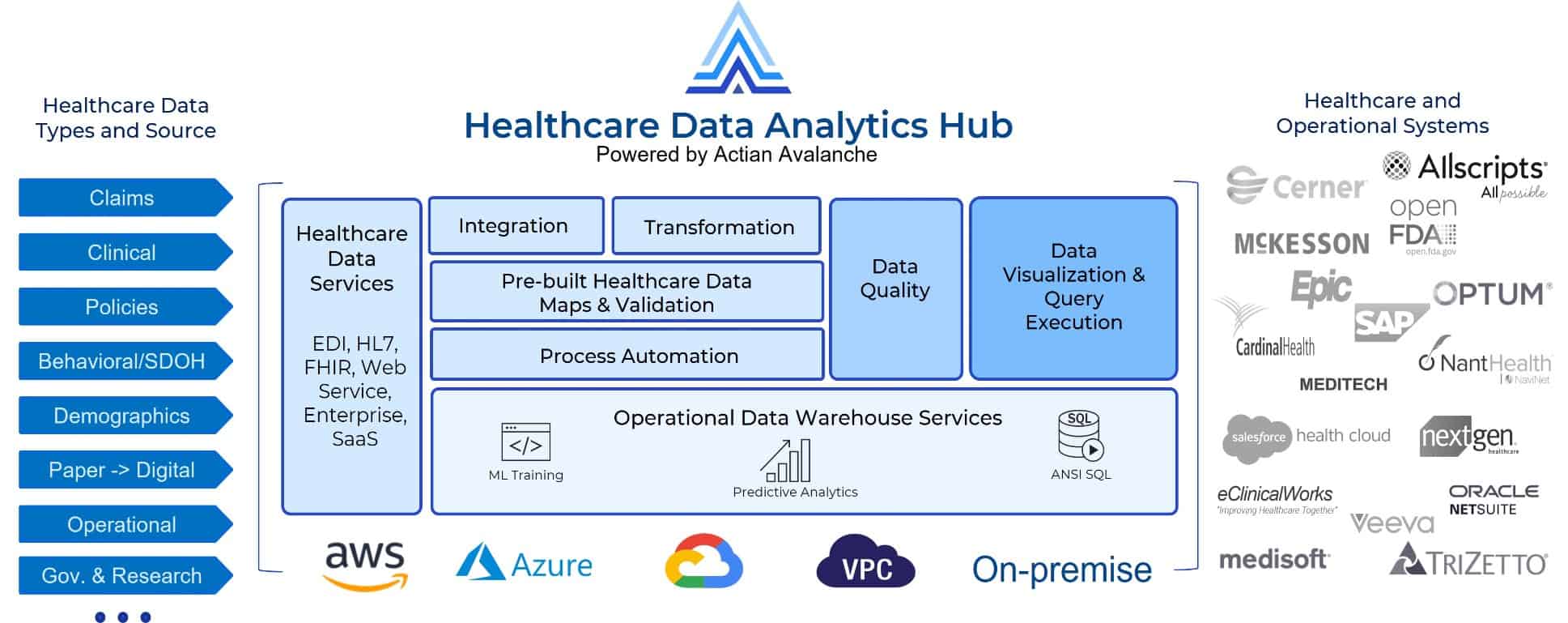
Provides self-service integration and built-in security features specific to healthcare data integration, management, and analytics.
Real-time insights across silos
Enables analysts and others outside IT to run analytics without perturbing the raw data, meeting HIPAA and other regulations.
Improve payer/provider alignment
Gain real-time insights across organizations to streamline operations, improve outcomes, and reduce costs.
OnDemand healthcare analytics webinar
What’s a Healthcare Data Analytics Hub and Why it Matters for Value-Based Care and Business Models?
Hosted by Actian and Chilmark Research

Real-time decision-making support with the Actian healthcare data analytics hub
View Data SheetThe healthcare transformation inflection point is here
In the wake of COVID-19, continually rising healthcare costs, and a rapidly changing market landscape, the need to pivot from reactionary, fee-for-service, in-person focused healthcare delivery to a value-based care and payments with shared risk, improved alignment, and transparency between payers and providers is imperative. This shift requires that the following five priorities be front and center post-pandemic:
- Adopt data integration and management platforms that support new CMS interoperability mandates.
- Securely share data across clinical, administrative, financial, and external population health and SDOH data silos.
- Build out patient and partner experience platforms that embrace the consumerization of healthcare.
- Streamline and make transparent key financial and operational core systems such as claims processing and revenue cycle management.
- Proactively identify and address error, abuse, and fraud.
What can a healthcare data analytics hub do for you?
Healthcare organizations need more accurate insights in real-time. With Actian they can quickly leverage the cloud to access and enrich, process and analyze, automate and act on the broadest set of healthcare data, empowering healthcare data analysts with self-service data integration and analysis, without impacting existing systems of record, and lowering the burden on IT.
Improve accuracy and accelerate reimbursements and claims processing
Value-based care requires value-based payments but, for this pairing to work, providers and payers must be aligned on a trusted and verifiable set of insights derived from more than just the transactional data at hand.
Reduce costs and time to onboard members, providers, and patients
Whether it’s patient admission to an ER, adding new hospital suppliers, or a new in-network provider for a payer, the ability to accurately gather the right information in real-time is critical to cost avoidance, improved care delivery outcomes, and alignment across all concerned parties.
Optimize network interoperability to support value-based care
Healthcare data silos generate a broad range of negative outcomes, ranging from medical errors and adverse drug reactions to simple yet frustrating repetition of re-entering the same information over and over. CMS and OHT have mandated an end to “walled gardens” and interoperability standards are eliminating excuses. However, the key to delivering value-based care and payments is as much about analysis and decision making once that data is shared as the sharing of the data itself.
Proactive error, abuse, and fraud detection and risk reduction
With the complexity of medical procedures, variety of goods and services, medical billing is prone to errors and waste. However analytics can tackle not only deliberate fraud but also unintentional errors, inefficiencies, and abnormal patterns and outliers.
Gain revenue cycle and operational insights
Gaining insights into revenue cycle patterns to better plan and forecast are essential in reduce claim rejections and denials while ensuring predictable revenue, sustained over a longer period of time through opportunities for shared risk and improved satisfaction rates between payers, providers and patients.
Build and sustain a Member360 view
Payers and managed care organizations must intelligently act on tailored member insights in real-time to effectively compete. In addition, Government mandates around medical price transparency, data interoperability, and the looming requirements around managing a person’s consent to share their personal health data make “member-360” initiatives an immediate imperative.
